45 M with Abdominal distension and b/l lower limb swelling
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings investigations and come up with diagnosis and treatment plan.
Unit 1
AMC bed 5
DOA:29/5/23
45 year old male ,lorry driver by occupation,resident of Nalgonda came to the opd with chief complaints of
Abdominal distension since 4-5 days
Abdominal bloating since 4-5 days
Shortness of breath since 4-5 days
Vomitings since 3 days
B/L lower limb swelling since 15-20 days
HOPI :
he was apparently asymptomatic 15 days back then he developed swelling of both lower limbs (extending up to knee ,pitting type)insidious in onset ,gradually progressive, no aggravating and relieving factors .
Abdominal distension since 5 days ,insidious in onset ,gradually progressive,no aggravating and relieving factors Associated with bloating ,SOB and vomitings
No h/o chest pain ,orthopnea ,PND,palpitations
No h/o deceased urine output,burning micturition ,fever
Past history
K/c/o DM since 4-5 years on medication Tab Metformin 500mg po BD
N/k/c/o HTN CVA CAD TB EPILEPSY
H/o Alcoholism since 10 years aggrevated 4 yrs back (180ml per day)
Personal history:
Diet :mixed
Appetite:normal
Bowel and bladder:regular
Sleep: adequate
Addictions:chronic alocoholic since 10years
No known allergies
Family history:not significant
General examination:
She is conscious,coherent , cooperative
Well oriented to time ,place and person
Vitals:
Temp:101.5F
Bp:130/70mmofhg
PR:119bpm
RR:20cpm
Grbs:mg/dl
No clubbing ,cyanosis, lymphadenopathy
CVS:s1s2+,no murmur
RS:BAE+,no added sounds
P/A:
Inspection;
Shape of abdomen; distended
Position of umbilicus: central and inverted
No scars and sinuses are present
All quadrants are moving equally with respiration
Palpation:
No tenderness
No organomegaly
Auscultation:
Bowel sounds heard
CNS: NFD
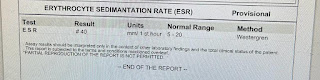
Investigations
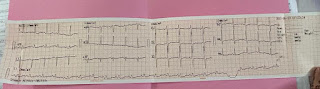
ECG
















Comments
Post a Comment