A 75 YR OLD MALE WITH SOB AND FEVER WITH CHILLS AND RIGOR
A 75 YR OLD MALE WITH SOB AND FEVER WITH CHILLS AND RIGOR
This is an online e log book to discuss our patient de-identified health data shared after taking his / her /
guardians signed informed consent. Here we discuss our individual patients problems through series of
inputs from available global online community of experts with an aim to solve those patients clinical
problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the
comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis"
to develop my competency in reading and comprehending clinical data including history, clinical findings
investigations and come up with diagnosis and treatment plan.
A. RAJKUMAR 7th Sem Roll 08
A 75 yr old male came with c.c of SOB (grade 3) since 3 hrs, loose stools 3 episodes, fever
with chills and rigors since 6 days.
H/O PRESENT ILLNESS: A 75 year male patient mason by occupation was a chronic smoker and alcoholic.
He used to smoke 18 beedis/day for 30 years and 90ml of alcohol per day. He was then diagnosed with TB for
which he took treatment for 2 years and stopped smoking , drinking regularly.But he then started taking
occasionally on family gatherings.
Due to repeated episodes of falls he went to govt hospital where the cause was identified to be low BP.
After 5 months he was diagnosed with high BP and started taking medications.
Patient had pedal edema 1 year back , so he came to KIMS and diagnosed with Renal failure and was
put on conservative treatment for 4 months followed by medication till now.
Patient had a h/o fall 1 week back and abrasion to head without loss of consciousness.
Patient is having low grade, intermittent fever for 2 days which relieved on medication. He has constipation
for which dulcoflex was given and then he had loose stools about 3 episodes from 3 hours.
pt is having SOB (grade 3 ) and became irritable.
PAST HISTORY ;
No similar complaints in the past.
H/O Hypertension and TB
TREATMENT HISTORY:
Diabetes: No
HTN: Yes
CAD: No
Asthma: No
TB: Yes
Antibiotics: No
Hormones: No
Chemo/Radiation: No
Blood transfusion: No
Surgeries: No
PERSONAL HISTORY:
Married
Appetite is Normal
Mixed diet
Bowel and bladder movements are regular
Micturition : Normal
No Known Allergies
Habits : Alcohol occasionally
FAMILY HISTORY:
Diabetes: No
HTN: No
Heart Disease: No
Stroke: No
Cancer: No
TB: No
Asthma: No
Any other hereditary diseases: No
Psychiatrist: No
Sibling History: No
Any other: No
PHYSICAL EXAMINATION:
GENERAL EXAMINIATION
Height
Weight
BMI
Body surface area
Pallor: present
Icterus: absent
Lymphadenopathy: absent
Clubbing of fingers: absent
Edema: absent
Malnutrition: No
Dehydration : No
VITALS
Temperature: 98.4 F
Pulse rate: 92/min
Respiration rate 22/min
BP: 150/70 mmhg
SPO2 at room air 90%
GRBS: 120 mg%
SYSTEMIC EXAMINATION
CARDIO VASCULAR SYSTEM
Thrills: No
Cardiac Sounds: S1,S2 heard
Cardiac murmurs: No
RESPIRATORY SYSTEM
Dyspnoea: No
Wheeze: Yes
Position of Trachea: Central
Breath Sounds: Vesicular
Adventitious Sounds: Rhonchi
ABDOMEN:
Shape of Abdomen: Scaphoid
Tenderness: No
Palpable mass: No
Hernial Orifices: Normal
Free Fluid: No
Bruits: No
Liver: Not palpable
Spleen: Not palpable
Bowel sounds: No
Genitals: Normal
Speculum Examination : Normal
PV Examination : Normal
P/R examination: Normal
CNS:.
Level of Consiousness: Consciousness/Alert
Speech: Normal
Signs of Meningeal irritation: No neck stiffness and Kerning's sign.
Cranial Nerves: Normal
Sensory System: Normal
Motor System: Normal
Glasgow Scale: 1
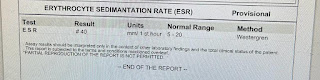
INVESTIGATIONS:
Hemogram
RBS
Serum electrolytes
LFT
ABG
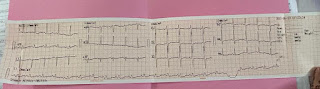
ECG








Comments
Post a Comment