76 year old female with hemiballismus secondary to uncontrolled sugars
This is an online e log book to discuss our patient de-identified health data shared after taking his / her /
guardians signed informed consent. Here we discuss our individual patients problems through series of
inputs from available global online community of experts with an aim to solve those patients clinical
problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the
comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis"
to develop my competency in reading and comprehending clinical data including history, clinical findings
investigations and come up with diagnosis and treatment plan.
Unit 1
Amc bed 1
DOA 22/5/23
A 66 yr old female ,residence of nalgonda came to the opd with c/o
Slurring of speech since 15days
Involuntary movements of right upper limb since 10days
And right lower limb since 5 days
She was apparently asymptomatic 15days ago then she developed swelling of tongue f/b slurring of speech , insidious in onset and gradually progressive,no aggravating and relieving factors
Not associated with deviation of mouth
C/o involuntary movements of right upper and lower limb,insidious in onset and gradually progressive , aggravating on increasing sugars and decreasing with decrease in grbs levels
She also c/o skin lesions over genital region since 15days
Past history:
K/c/o HTN since 2 years
K/c/o DM since one week
She has h/o joint pains( shoulder and elbow) since 2-3 months for which she went to a local hospital and the reports shower RA FACTOR+
and was advised tab . methotrexate (on regular medication)
Personal history:
Diet :mixed
Appetite:normal
Bowel and bladder:regular but c/o burning micturition since 1 month
Sleep: adequate
Family history:not significant
General examination:
She is conscious,coherent , cooperative
Well oriented to time ,place and person
Vitals:
Temp:98.6F
Bp:120/70mmofhg
PR:118bpm
RR:20cpm
Grbs:339mg/dl
No pallor ,icterus ,clubbing ,cyanosis ,lymphadenopathy and edema
CVS:s1s2+,no murmur
RS:BAE+,no added sounds
P/A:
Inspection;
Shape of abdomen; obese
Position of umbilicus: central and inverted
No scars and sinuses are present
All quadrants are moving equally with respiration
Palpation:
No tenderness
No organomegaly
Auscultation:
Bowel sounds heard
CNS:
Motor system:RIGHT b LEFT.l Left
Tone :UL: N. N
LL: N. N
Power:UL: 4/5 4/5
LL: 3/5 4/5
Reflexes:
Biceps:
Triceps :
Supinator:
Knee:
Ankle:
Plantar : flexion
Obg referral taken I/v/o reddish skin lesions over vulva and inner groin region,white discharge since 15days.
Diagnosis: 66year old p5L5 post hysterectomised with DM 2 and HTN with genital lesions
Advised :
1.inj.ceftrioxone 1gm iv stat f/b Tab.erythromycin 500mg po/BD
2.T.pantop 40mg po/OD
3.T.metronidazole 400mg po/TID
4.Antibiotic dosage can be escalated or deescalated after swab c/s report
Dvl referral taken I/v/o genital ulcer :
Diagnosis:Genital ulcer for evaluation+vulvo vaginal candidiasis
Advised :
1.clotrimazole 1%cream L/A BD for 1 week
2.Tab.BACT ointment L/A BD for 1 week
Review referral:
Diagnosis:Genital ulcer for Evaluation
?Frictional ulcer
?herpes genitalis + vulvovaginal candidiasis
Advised:
1.1.clotrimazole 1%cream L/A BD for 1 week
2.Tab.BACT ointment L/A BD for 1 week
3.continue same treatment as advised by physician
Opthalmology referral taken I/v/o HTN and DM retinopathy changes :
Impression: no diabetic and HTN retinopathy changes noted in both eyes.
Provisional diagnosis:
Right Hemiballismus secondary to ?Type II DM ?Basalganglia lesion
Hypokalemia Secondary to
?GI Losses ?Nutritional
Genital ulcer for Evaluation
?Frictional ulcer
?herpes genitalis + vulvovaginal candidiasis
K/c/o HTN 2yrs
Denovo DM-II (one week)
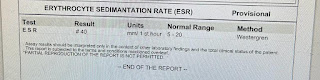
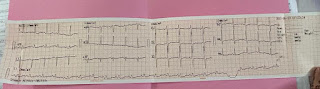
Investigations:
Serology :negative
Chest xray:
USG abdomen:
ECG:
Treatment:
IVF NS and RL @75ml/hr
Inj.optineuron 1amp in 100ml Ns /iv/OD
Tab .amlodipine 5mg po/OD
Tab.tetrabenzine 25mg/poBD
Tab.metrogyl 400mg/po/TID
Tab.pan 40Mg po/OD
Tab.sporolac-Ds po/TID
Inj.HAI sc/TID acc to grbs
Syp.potklor 10ml/po/BDwith glass of water
T.bact ointment for LA /BD
Clotrimazole 1%cream LA/BD
Capsule redotil 100mg po/BD
Advice at discharge:
Final diagnosis
Right Hemiballismus secondary to ?Type II DM ?Basalganglia lesion
Hypokalemia Secondary to
?GI Losses ?Nutritional
Genital ulcer for Evaluation
?Frictional ulcer
?herpes genitalis + vulvovaginal candidiasis
Acute Diarrhoea (Resolving)
K/c/o HTN 2yrs
Denovo DM-II (one week)
Discharge summary
A 66 yr old female ,residence of nalgonda came to the old with c/o
Slurring of speech since 15days
Involuntary movements of right upper limb since 10days
And right lower limb since 5 days
She was apparently asymptomatic 15days ago then she developed swelling of tongue f/b slurring of speech , insidious in onset and gradually progressive,no aggravating and relieving factors
Not associated with deviation of mouth
C/o involuntary movements of right upper and lower limb,insidious in onset and gradually progressive , aggravating on increasing sugars and decreasing with decrease in grbs levels
She also c/o skin lesions over genital region since 15days
Past history:
K/c/o HTN since 2 years
K/c/o DM since one week
She has h/o joint pains( shoulder and elbow) since 2-3 months for which she went to a local hospital and the reports shower RA FACTOR+
and was advised tab . methotrexate (on regular medication)
Personal history:
Diet :mixed
Appetite:normal
Bowel and bladder:regular but c/o burning micturition since 1 month
Sleep: adequate
Family history:not significant
General examination:
She is conscious,coherent , cooperative
Well oriented to time ,place and person
Vitals:
Temp:98.6F
Bp:120/70mmofhg
PR:118bpm
RR:20cpm
Grbs:339mg/dl
No pallor ,icterus ,clubbing ,cyanosis ,lymphadenopathy and edema
CVS:s1s2+,no murmur
RS:BAE+,no added sounds
P/A:
Inspection;
Shape of abdomen; obese
Position of umbilicus: central and inverted
No scars and sinuses are present
All quadrants are moving equally with respiration
Palpation:
No tenderness
No organomegaly
Auscultation:
Bowel sounds heard
CNS:
Motor system : RIGHT LEFT Tone :UL: N. N
LL: N. N
Power:UL: 4/5 4/5
LL: 3/5 4/5
Reflexes:
Biceps:
Triceps :
Supinator:
Knee:
Ankle:
Plantar : flexion
Obg referral taken I/v/o reddish skin lesions over vulva and inner groin region,white discharge since 15days.
Diagnosis: 66year old p5L5 post hysterectomised with DM 2 and HTN with genital lesions
Advised :
1.inj.ceftrioxone 1gm iv stat f/b Tab.erythromycin 500mg po/BD
2.T.pantop 40mg po/OD
3.T.metronidazole 400mg po/TID
4.Antibiotic dosage can be escalated or deescalated after swab c/s report
Dvl referral taken I/v/o genital ulcer :
Diagnosis:Genital ulcer for evaluation+vulvo vaginal candidiasis
Advised :
1.clotrimazole 1%cream L/A BD for 1 week
2.Tab.BACT ointment L/A BD for 1 week
Review referral:
Diagnosis:Genital ulcer for Evaluation
?Frictional ulcer
?herpes genitalis + vulvovaginal candidiasis
Advised:
1.1.clotrimazole 1%cream L/A BD for 1 week
2.Tab.BACT ointment L/A BD for 1 week
3.continue same treatment as advised by physician
Opthalmology referral taken I/v/o HTN and DM retinopathy changes :
Impression: no diabetic and HTN retinopathy changes noted in both eyes.
Treatment:
IVF NS and RL @75ml/hr
Inj.optineuron 1amp in 100ml Ns /iv/OD
Tab .amlodipine 5mg po/OD
Tab.tetrabenzine 25mg/poBD
Tab.metrogyl 400mg/po/TID
Tab.pan 40Mg po/OD
Tab.sporolac-Ds po/TID
Inj.HAI sc/TID acc to grbs
Syp.potklor 10ml/po/BDwith glass of water
T.bact ointment for LA /BD
Clotrimazole 1%cream LA/BD
Capsule redotil 100mg po/BD
Advice at discharge:






















Comments
Post a Comment