27 yr old male presented with stomach pain
27yr old male resident of vellanki Mason by occupation came with chief complaints of stomach pain since 2 days
An episode of vomiting just before presentation
HOPI:
Patient was apparently asymptomatic 3days ago then he developed stomach pain in epigastric area which is insidious in onset pricking and shooting type of pain radiating to back (lumbar region) gradually progressive in nature aggregated on not having food and no relieving factors
7-8 episodes of non projectile and non bilious vomiting
History of fever 10days ago
History of weight loss, loss of appetite, insomnia, fatigue
No complaints of chest pain, palpitations, SOB, headache, burning micturition,loose stools, giddiness
SEQUENCE OF EVENTS
PAST HISTORY
He is known alcoholic since 5 years with a daily intake of 160ml
No history of DM,TB, ASTHMA,HTN, EPILEPSY, THYROID DISORDERS, ALLERGIES
FAMILY HISTORY
No relevant family history
PERSONAL HISTORY
Diet mixed
Appetite reduced
Bowel and bladder movements regular
Addiction alcohol regular and smoke occasionally until 3yrs back
TREATMENT HISTORY
GENERAL PHYSICAL EXAMINATION
On examination, patient is conscious, coherent, cooperative
patient is moderately built and moderately nourished
No pallor,icterus, cyanosis, clubbing, lymphadenopathy, edema
Vitals
Fever chart
Temperature- afebrile
Pulse rate -64/min
Respiration rate-20/min
BP-130/100mm/Hg
SYSTEMIC EXAMINATION:
Abdominal examination:
Inspection
Umbilicus inverted , No abdominal distention,no visible pulsations,scars and swelling.
Palpation
Soft, non tender, no organo megaly.
Auscultation
Bowel sounds Heard
Cardio vascular examination:
No visible pulsations, scars, engorged veins. No rise in jvp
Apex beat is felt at 5 Intercoastal space medial to mid clavicular line.
S1 S2 heard . No murmurs.
Respiratory system :
Shape of chest is elliptical, b/l symmetrical.
Trachea is central. Expansion of chest is symmetrical
Bilateral Airway Entry - positive
Normal vesicular breath sounds
CNS examination: No neurological deficit found.
Gait: normal.
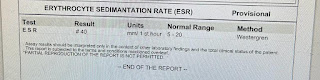
INVESTIGATIONS
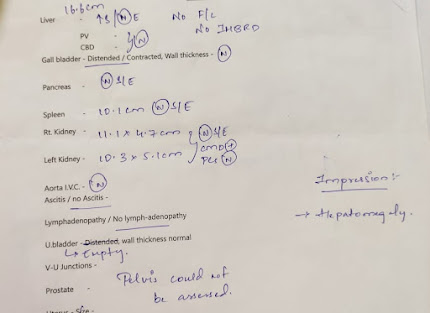
USG
Serum electrolytes
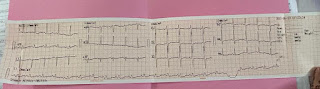
ECG
PROVISIONAL DIAGNOSIS
Alcoholic gastroenteritis
TREATMENT AND FOLLOW UP














Comments
Post a Comment