1801006001-Long case
This is an online E-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient centered online learning portfolio and your valuable comments on comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
60 YRS OLD MALE WITH THE COMPLAINTS OF UPPER AND LOWER LIMB SWELLING SINCE 10 DAYS
Chief complaints:
A 60 year old gentleman came to the casualty with the cheif complaints of edema of both upper and lower limbs since 10 days,complaints of facial swelling decreased urine output since yesterday, vomiting of 6 episodes on 11/03/23(Saturday), loose stools of 4 episodes on 12/03/23(Sunday) morning.
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic 10 days back then he developed Bilateral pedal edema since 10 days which was insidious in onset and gradually progressive in nature for which he admitted in government hospital. Condition worsened and swelling of face bilateral upper limb started 4 days back .
Complaints of decreased urine output on day before presentation
Associated with 6 episodes of vomiting food particles as content non bilious non projectile non blood tinged
4 episodes of loose stools watery non blood stained
No history of fever, palpitations, sob, pain abdomen, sweating, burning micturition
SEQUENCE OF EVENTS;
18 Yrs back after his sister's death he was deprived emotionally and haven't had food for 2-3days and suddenly became altered and passed stools invoultarly for this complaints patient was brought to hospital and diagnosed with type2 DM and was on OHA and insulin from then.
↓
8yrs back he met with an accident and had fracture of right shoulder for which he underwent a surgery.
↓
Around 6 years back, one fine day when he went to pass urine, patient suddenly had LOC for around 10 mins with involuantry movements of ?Rt Upper limb and lower limb, uprolling of eyes + , tongue bite + frothing from mouth + and he was taken to local hospital where they were said to have to significant findings in CT and he hasn't been started on any medications and sent to home with in 2-3 days.
↓
4yrs back when he was working while cutting trees a log fell on his right lower limb and had fracture of right NOF and right knee for which open reduction and internal fiation was done and he has't been working since then he also diagnosed to have hpertension.
↓
2yrs back patient developed altered sensorium and was having hyperglycemia at private hsptl then he was diagnosed to have DKA and treated with inslin.
↓
4 months back he complained of pedal edema for which they went to nalgonda hsptl and stayed approximately 1 week and resolved edema ,while planning for discharge he suddenly developed vomitings for 3days (non bilious, non projectile vomitings) later on his sensorium deteriorated and aphasia also developed and brought to our hsptl and found out to be having hyponatremia and hypokalemia and corrected with 3%NS and later with in 1-2 days patient became normal and thought of SIADH secondary to ?frontal lobe contusion and he was discharged with normal electrolyts.
↓
10 days back (6/3/23) patient developed pedal edema for which he went nalgonda hsptl again and treated there for 4days and on 10/3/23 he suddenly started having vomitings(6 episodes of vomitings in 2 days) and loose motions (7 episodes in 2 days) later on his sensorium deteriorated and brought to our hsptl on sunday night(12/3/23).
Bilateral pedal edema
Past history:
History of similar complaints in the past and admitted in the hospital on 23rd December 2022 and discharged on 31 December 2022. There was history of altered sensorium present at the time of previous hospitalisation.
Known case of diabetes from 18 years. On Tab. Glimipride 1mg before breakfast and Tab. Metformin 500 mg after breakfast.
Known case of hypertension since 4 years. On Tab. Telma H(TELMISARTAN 40 mg+ hydrochlorthiazide 12.5mg) in morning and Tab. Cilacar 10mg at night.
Not a known case of tuberculosis, bronchial asthma, CAD, CVD.
PERSONAL HISTORY:
Farmer by occupation. Stopped since 4 years
Appetite decreased from 10 days
Decreased urine output since yesterday
Known alcoholic. Stopped from 20years
Known smoker stopped since 20 years
DAILY ROUTINE OF PATIENT:used to wake up at 6 am and will do his morning rituals by 7:30 am
and will have breakfast by 8 amwhich consists of rice,curry and goes to work he used to do ctting trees and woods also sometimes he goes to his own feileds where he waters the fields and removes the weeds sowing fertilisers and some cattle rearing too and will have his lunch by 1 pm which consists of rice ,curry and comes to the home by 5 or 6 pm and will freshens up and will have dinner by 8pm and goes to bed by 10pm.
GENERAL PHYSICAL EXAMINATION:
Patient is conscious coherent and cooperative well oriented to time place person
Moderately built and moderately nourished.
No signs of pallor, icterus, cyanosis, clubbing, generalised lymphadenopathy
VITALS:
TEMPERATURE: 97.4°F
PULSE RATE: 90bpm
RESPIRATORY RATE: 18cpm
BLOOD PRESSURE: 140/80mm Hg
SPO2: 97% @ Room air
GRBS:306mg/dl
SYSTEMIC EXAMINATION:
CARDIOVASCULAR SYSTEM:
Inspection :
Shape of chest- elliptical shaped chest
No engorged veins, scars, visible pulsations
No raised JVP.
Palpation : Apex beat can be palpable in 5th inter costal space medial to mid clavicular line.No thrills and parasternal heaves can be felt
Auscultation : S1,S2 are heard ,no murmurs.
RESPIRATORY SYSTEM:
Inspection: Shape of the chest : elliptical ,B/L symmetrical ,
Both sides moving equally with respiration
No scars, sinuses, engorged veins, pulsations
Palpation:Trachea - central
Expansion of chest is symmetrical.
Auscultation:
B/L air entry present . Normal vesicular breath sounds.
CENTRAL NERVOUS SYSTEM:
Conscious, oriented to time place and person.
GCS on the day of admission was E4 V5 M6
speech : normal
Behavior : normal
Memory : Imediate memory is slightly impaired recent and remote memory is intact.
No hallucinations or delusions
CRANIAL NERVE EXAMINATION:
1st : Normal
2nd : normal
3rd,4th,6th : normal
5th : sensory intact
7th :no abnormality noted
8th : No abnormality noted.
9th,10th : palatal movements present and equal.
11th,12th : normal.
MOTOR SYSTEM EXAMINATION
Bulk of the muscle: normal
Tone of muscle : normal
POWER -
RT. LT
Upper limb 3/5. 3/5
Lower limb 4/5. 4/5
SUPERFICIAL REFLEXES :
corneal ,conjunctival ,plantar reflexes are present
DEEP TENDON REFLEXES :
BP TRI SUP KNEE ANK PLAN
RT ++ + + ++ ++ ++ Flex
LT ++ ++ ++ ++ ++ Flex
SENSORY SYSTEM EXAMINATION
SPINOTHALAMIC SENSATION
Crude touch normal
Pain normal
DORSAL COLUMN SENSATION
Fine touch normal
Proprioception normal
CORTICAL SENSATION
Two point discrimination able to discriminate
Tactile localization able to localize
CEREBELLAR SIGNS : no
Meningeal signs: no
PER ABDOMEN: soft non tender.
Inspection:on inspection abdomen is flat, symetrical,and not distended.umbilcus is centre and inverted.no scars,engorged veins are seen.All 9 regions of abdomen are equally moving with respiration.all hernial orfices are clear.
Palpation:on palpation abdomen is soft , no tenderness no other palpable organs are felt.On bimanual examination of kidney is not palpable.All inspectory findings are confirmed.
percussion:no shifting dullness, no fluid thrills.
auscultation:normal bowel sounds are heard.
INVESTIGATIONS:
CHEST X RAY:
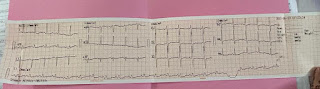
ECG:
2D ECHOCARDIOGRAPHY:
TRIVIAL TR+/AR+: NO MR
NO RWMA. NO AS/MS. SCLEROTIC AV
GOOD LV SYSTOLIC FUNCTION
DIASTOLIC DYSFUNCTION. NO PAH
ULTRASOUND:
IMPRESSION:
BILATERAL RENAL CORTICAL CYSTS
BILATERAL RAISED ECHOGENECITY OF KIDNEYS
INCREASED URINARY BLADDER WALL THICKNESS
CORRELATE WITH CUE TO RULE OUT CYSTITIS
HEMOGRAM
Hb 9.5gm/dl
Total count 11500cell/cumm
Neutrophils 91%
Lymphocytes 6%
Pcv 24.7vol%
Mcv 76 fl
MCHC 38.5%
RBC 3.25 millions/cumm
SERUM ELECTROLYTES
12/03/23ABG
SERUM CREATININE
1.5mg/dl (0.9-1.3)
COMPLETE URINE EXAMINATION
BUN/CREATININE: 12.6
PROVISIONAL DIAGNOSIS:
HYPOOSMOLAR HYPERVOLEMIC HYPONATREMIA WITH HYPOKALEMIA WITH ACUTE KIDNEY INJURY(RENAL) WITH K/C/O DIABETES AND HYPERTENSION WITH MILD ANEMIA
TREATMENT:
1. FLUID RESTRICTION
2. INJ. KCL 20mEq IN 100ML NS @ 20ml/hr
3. TAB. METFORMIN 500 MG PO/BD
4. TAB. GLIMIPERIDE 1MG PO/BD
5. TAB. TELMA 40 MG PO/BD
6. TAB. MET XL 25 MG PO/BD
7. VITALS MONITORING
8. 7 POINT GRBS MONITORING.
9.TAB. CILINDIPINE 10MG PO/BD
10. INPUT OUTPUT CHARTING
11. SYRUP. POTCHLOR 15ML PO/TIDVIN 1 GLASS OF WATER
12. INJ. ZOFER 4 MG IV/SOS
13. INJ. PAN 40 MG IV/OD
14. TAB. ALDACTONE 50 MG PO/OD
15. TAB. GLICLAZIDE 40 MG PO/OD










Comments
Post a Comment